Taiwan’s hospitals fighting the COVID-19 blues

Source:Chien-Ying Chiu
In 2020, Taiwan was considered the gold standard for handling COVID-19. Now, a sudden surge in cases has stretched medical resources in the Greater Taipei area to their limits, leaving many to wonder how long it will take to bring this spike under control.
Views
Taiwan’s hospitals fighting the COVID-19 blues
By Pei-hua LuCommonWealth Magazine
♦ Updated daily |Taiwan’s Covid-19 Outbreak
The COVID-19 outbreak has engulfed the Greater Taipei area in northern Taiwan, forcing life and death to live side-by-side.
“I never thought home isolation meant holding a funeral,” said KK, a family member of a COVID-19 victim.
Though KK’s 80-year-old uncle had chronic illnesses, they were kept under control with medication, and he remained active, regularly going to the market and meeting up with friends. In early May, KK’s family got word that her uncle had come in contact with a person who tested positive for COVID-19 and needed to be isolated at home.
Because the family’s home had two bathrooms, the uncle lived by himself in a room with its own bathroom. He would call family members living in the rest of the apartment daily to tell them he was doing fine. He never ran a fever.
Suddenly, on the final day of the 14-day quarantine, the uncle’s condition took a turn for the worse. The family called an ambulance, but after waiting three hours to no avail, they decided to rush the uncle to a nearby hospital themselves, and he died there a day later. It was only a day after the man had passed away that the hospital told the family he had been infected with COVID-19.
What most angered the family was how quickly everything happened at the end. They had connected with the uncle by video conference the morning he died, only to get the bad news from the hospital that night, and the hospital insisted that the body be cremated within 24 hours. Family members who lived in the same apartment as the uncle, however, were consigned to home isolation, and could not handle any of the arrangements themselves.
“Everything just went way too fast, to the point where we had no time to react,” KK said.
When news of COVID-19 deaths had been reported in the past, it had meant little to KK or her relatives. Now that the uncle’s “isolation” became permanent, however, they realized how serious the situation was.
Taiwan had reported fewer than 200 domestically transmitted COVID-19 cases from when COVID-19 emerged in January 2020 to early May 2021, but more than 7,100 cases were added to that number in just 17 days from May 15, when the current spike began, to May 31.
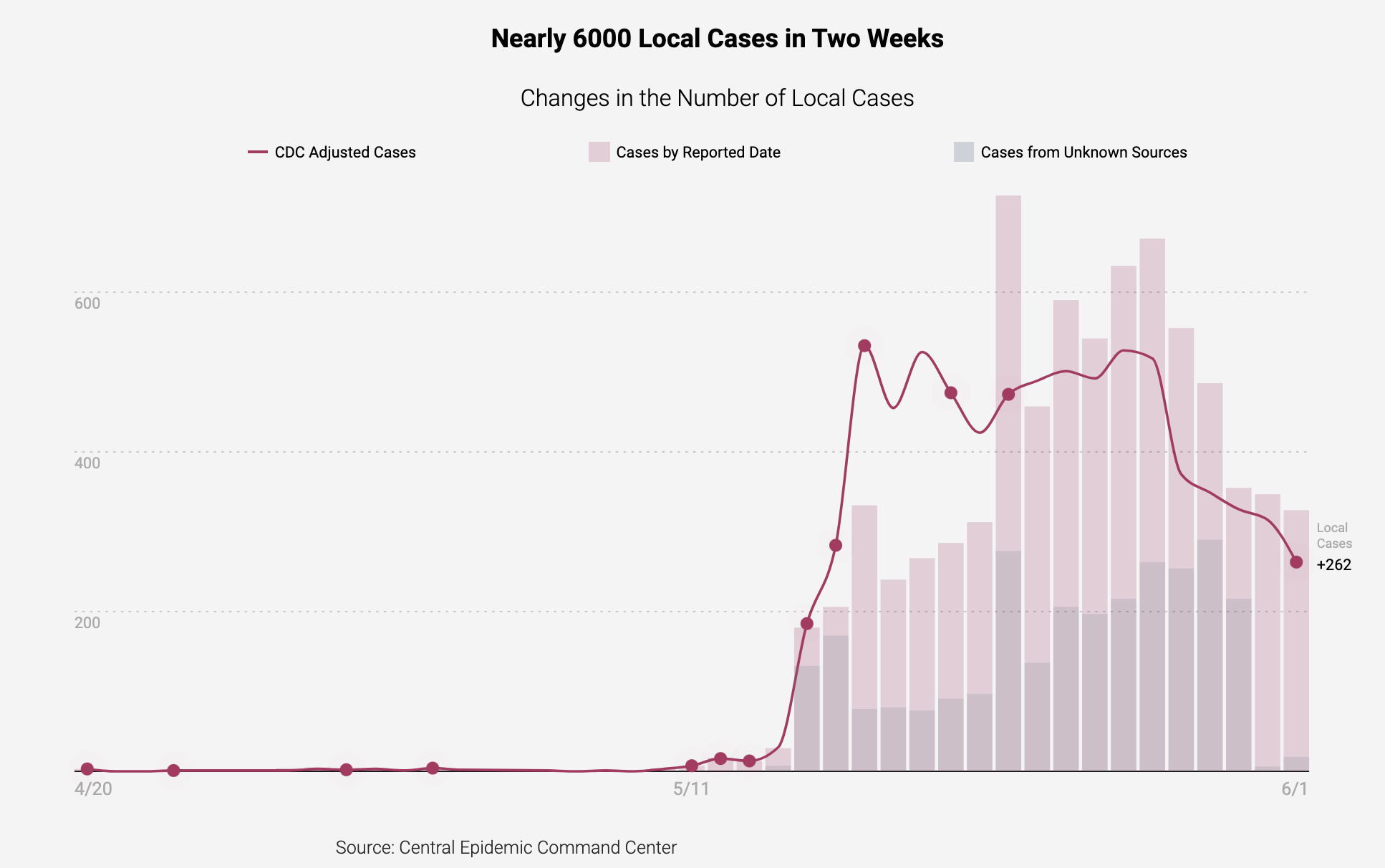 Nearly 6000 local cases in two weeks. (Source: CommonWealth Magazine)
Nearly 6000 local cases in two weeks. (Source: CommonWealth Magazine)
This sudden surge revealed to a population largely isolated from the disease for over a year how fierce it can actually be, and older people with chronic illnesses have been the hardest hit.
According to Taiwan CDC statistics, less than 10 percent of COVID cases in 2020 were classified as severe, but that has risen to nearly 20 percent for those 60 and over in the latest wave of cases.
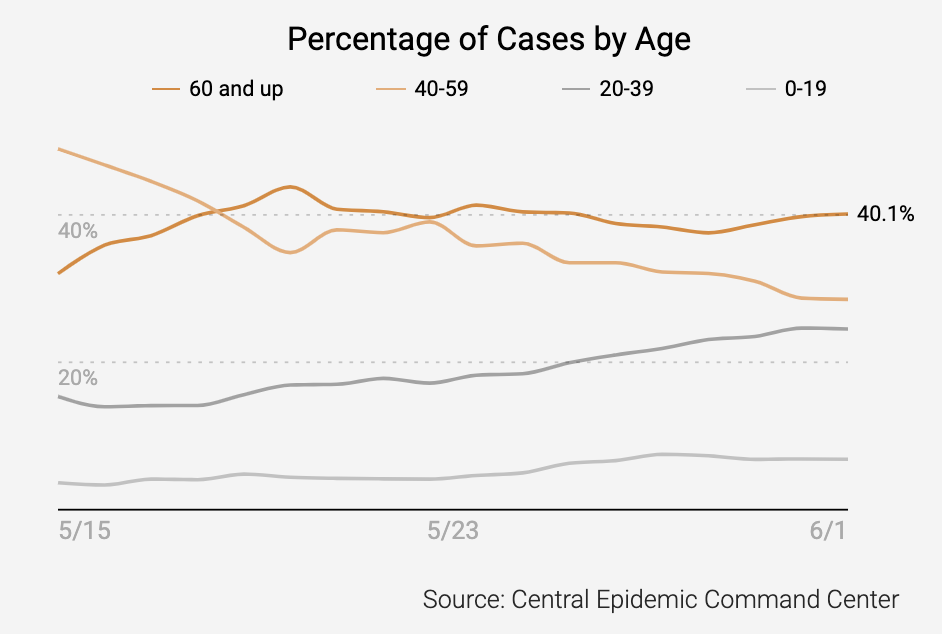
High percentage of elderly cases. (Source: CommonWealth Magazine)
The number of people in home isolation has soared, yet in many cases they have no way of getting a COVID-19 diagnosis quickly even if they may have the disease. Several people have been confirmed as having COVID-19 only after they died, reflecting a medical system – from hospitals and testing stations to ambulances – in which demand for services has outstripped supply.
The sharp rise in severe cases is squeezing medical resources to the brink, particularly in Taipei and New Taipei cities where the latest outbreak has been concentrated.
Scenario 1: National Taiwan University Hospital emergency room
On the night of May 26, National Taiwan University Hospital (NTUH) Superintendent Wu Ming-shiang sent out a plea for help on his Facebook page titled “Hospitals Need Help!”
NTUH and its children’s hospital have 32 negative pressure rooms combined. Three are for the exclusive use of newborn babies, leaving 29 for other uses, and those were quickly filled in the latest surge.
NTUH Vice Superintendent Lai I-rue said ambulances have been delivering COVID-19 patients to the hospital after striking out at other facilities, and NTUH has taken them in despite not having any beds available, because rejecting them would immediately make the news and send a bad message.

(Source: Pei-Yin Hsieh)
Speaking with a sad smile, he said his greatest fear every day was getting a call at around 8-9 p.m., because it usually meant there was a problem in the emergency room.
Of the more than 90 severe COVID-19 patients in Taiwan on ventilators, NTUH has admitted nearly one-fifth of them, CDC statistics show. Some were originally the hospital’s patients, but many were transferred there from government quarantine centers or quarantine hotels as mild cases turned into medium and severe cases.
NTUH is not the only hospital under pressure. Several hospitals in the Greater Taipei area have been on the verge of differing degrees of collapse.
Scenario 2: Ambulances with nowhere to go
As the COVID-19 pandemic raged around the world last year, Taiwan was largely unscathed and its medical services untested. When an ambulance service was notified that a COVID-19 patient needed help, health departments had already arranged the hospital where the individual would go. The patient could be taken to the hospital’s basement by ambulance personnel and then sent directly to their rooms, eliminating any unnecessary contact with other people.
But those days are gone.
Now, when ambulance responders arrive at a patient’s home, they often have no idea where the patient should be taken to and end up waiting with the family for instructions from health authorities. Even if the patient makes it into the ambulance, hospitals often respond that their beds are full, forcing the ambulance to drive around the city looking for an opening. And even if a hospital grudgingly admits the patient, the individual will likely face a one- to two-hour wait after registering before a doctor can see them.
 (Source: Chien-Ying Chiu)
(Source: Chien-Ying Chiu)
“Right now, almost every hospital is providing first aid outdoors, but they still cannot absorb the rapidly increasing number of severe COVID-19 cases,” said Hou Sheng-wen, an attending physician in Shin Kong Wu Ho Su Memorial Hospital’s Emergency Department.
None of these problems happen in isolation. The shortage of negative pressure rooms and dedicated rooms for COVID-19 patients means that severe cases sent to emergency rooms have nowhere to go and take up emergency room resources, which in turn leaves hospitals unable to admit severe cases brought to them by ambulances.
Huang Li-min, an infectious disease specialist who heads NTUH’s Department of Pediatrics, noted bluntly that hospitals dependent on Taiwan’s national health insurance system for their income already had relatively streamlined staffs, and those staffs have now been stretched beyond their limits by the surge in patients, he said.
To help the situation, the CDC has announced measures to send some patients to hospitals south of Greater Taipei and allow more than one patient per room, but frontline medical workers remain skeptical, Huang said. The only patients being sent south at present are new cases, and only a fraction of them at that, indicating that Taipei hospitals will continue to see their burdens rise.
Hou said the only solution is for patients to be sent south on a rotating basis to give each facility some breathing room.
The vaccination gap
Most experts believe the only way to ultimately quell the outbreak is to vaccinate Taiwan’s population, but increasing the vaccination rate poses major challenges in the short term.
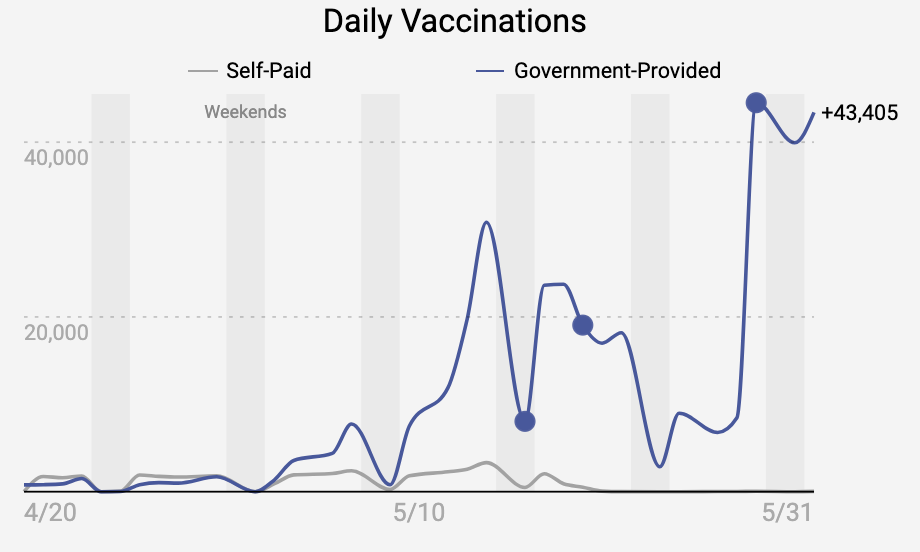
Increasing vaccinations. (Source: CommonWealth Magazine)
As of the end of May, Taiwan had received a total of 876,000 vaccines, with about 560,000 of them coming in the last two weeks of May, still a long way away from the number needed for a population of 23.5 million people. Health Minister Chen Shih-chung said on May 28 he did not expect 60 percent of the population (where some experts believe herd immunity can be achieved) to get even a first vaccine shot until October.
“The vaccination rate right now is very low and cannot do much to stop community transmissions. It will only help control nosocomial [hospital-acquired] infections,” said Chen Hsiu-hsi, a public health professor at NTU.
Chen believed, however, that the recent surge in cases could be contained and the Level 3 alert imposed on May 17 could be lifted around mid-June if people stick to what has been a soft lockdown.
No gatherings = lower infection rate
The Level 3 alert requires people to avoid indoor gatherings of more than five people and outdoor gatherings of 10 people. In practice this has meant a shutdown of eight types of entertainment businesses and public venues, a suspension of in-restaurant dining, and school closings.
Government officials have even urged people to follow the core of Level 4 guidelines – do not go out unless necessary – but have not opted for the most restrictive Level 4 measure – a full lockdown.
NTU’s Chen has long monitored changes in data on nonpharmaceutical interventions (NPI) – actions other than getting vaccinations or taking medicine that can slow the spread of disease – and he believed the trigger of the recent spike in cases occurred around Mother’s Day on May 9 when many Taiwanese let down their guard.
At that time, almost nobody wore masks, whether at family gatherings or in the teahouses with hostesses in Wanhua District, seen as the epicenter of the recent spike, Chen said. Those interactions caused the overall protection efficacy of NPIs in society, whether through government mandates or individual practices, to drop from 70 percent to 45 percent.
Now that the Level 3 alert is in place, that protection level has risen back up to 75 percent, but while a level of 70 percent was high enough to keep COVID-19 at bay last year, it will take a 90 percent efficacy rate to contain the more potent U.K. variant of the disease, Chen argued.

(Source: Chien-Ying Chiu)
Traditional markets and the so-called eight types of businesses that have been shut down will be the keys to whether the coronavirus is contained or is reignited, he said.
If the epidemic were to spin out of control and merge with the fall and winter flu season, medical resources would come under even heavier pressure, potentially triggering panic.
Several experts contended that the virus is not at its most infectious during the hot summer months and that the next critical juncture will be in September. They warn that if Taiwan is not careful, the convergence of cooler weather, the flu and the virus could worsen the situation.
Hitting home
The medical chaos and shortfall of resources caused by the spread of COVID-19 have hit home with people in Taiwan, especially those living in the Greater Taipei area.
 (Source: Chien-Tong Wang)
(Source: Chien-Tong Wang)
“Hospitals are about to collapse. If you can stay at home and take care of yourself, then do it,” said KK, issuing a fervent appeal to all of society to take the situation seriously.
Still thinking of her loss, KK now implores her elders not to go to traditional markets anymore. Also, after buying a blood oxygen monitor at a local pharmacy, she tracks her temperature and blood oxygen level every day, reflecting the urgency that many people in Taiwan now feel in fighting COVID-19.
Have you read?
♦ Updated daily |Taiwan’s Covid-19 Outbreak
♦ Infographics|Taipei Lockdown
♦ NTU expert: Taiwan doesn’t need lockdowns
Translated by Luke Sabatier
Edited by TC Lin
Uploaded by Penny Chiang






