On the trail of the COVID-19 vaccine Holy Grail
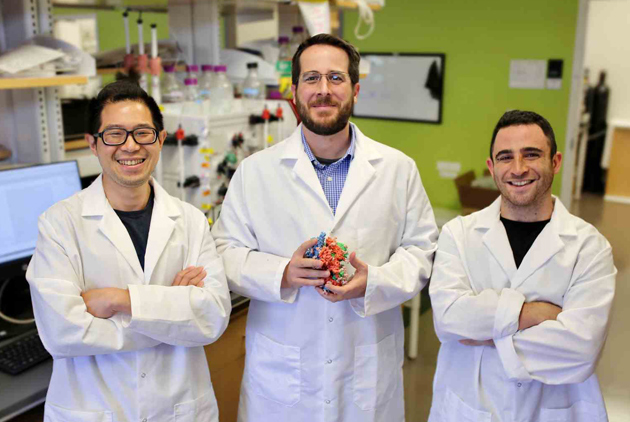
Source:Jason McLellan
Soon after COVID-19 erupted, a Texas university lab isolated proteins that helped U.S. companies develop vaccines in record time. It then came up with a potentially game-changing 2nd-generation protein, described in a study in which the lead author was Taiwanese. Here’s how they did it, and what it may mean.
Views
On the trail of the COVID-19 vaccine Holy Grail
By Ching Fang WuFrom CommonWealth Magazine (vol. 726 )
♦ How far is Taiwan from herd immunity?
The United States faced a major emergency early in 2020 when COVID-19 ruthlessly started taking people’s lives. While much of the country was shut down, however, a laboratory at the University of Texas at Austin was given special permission to continue its research.
Busy at work was Taiwanese postdoctoral researcher Hsieh Ching-lin (謝慶霖), who was combing through more than 100 microscopic spike proteins in search of a way to create a more effective, easier-to-produce vaccine for the COVID-19 virus – SARS-CoV-2.
His findings contributed to the development of a second-generation COVID-19 vaccine that is currently undergoing human clinical trials in Thailand, Vietnam, Brazil and Mexico. This new vaccine “could change how the world fights the pandemic,” the New York Times wrote in early April 2021.
“We feel that this vaccine could be the one that is used the most in the future,” Hsieh said in an interview with CommonWealth Magazine.
After graduating with a degree from National Taiwan University’s School of Veterinary Medicine, Hsieh got a master’s in biochemistry from Academia Sinica and then went to the United States to advance his career.
In searching for a pathway to a Gen 2.0 vaccine, Hsieh, his lab’s director Jason McLellan, a professor of molecular biosciences at the university, and other scientists were hoping to do more to rid the world of the scourge of COVID-19.
Hsieh and the team had already made it possible for companies and institutions to develop an effective first-generation vaccine against the disease in under a year’s time.
When COVID-19 first emerged outside of China in early 2020, the team designed a “spike protein” called “S-2P” that is now used in the Moderna, Pfizer-BNT, Johnson & Johnson, and Novavax vaccines and even the Taiwan-made Medigen vaccine to trigger an immune reaction.
Finding the right spike protein in just 2 weeks
What is a spike protein? They are the proteins that cover the surface of the COVID-19 coronavirus. Once these spikes attach themselves to human cell membranes, they open a pathway for the virus to attack the cell’s nucleus, in effect kidnapping human cells to spread the virus.
Theoretically, if you send a protein that looks identical to the SARS-CoV-2 protein into a human cell, the immune system will learn to recognize it, and then mount an immune response when it encounters the real virus.
The shape of the spike protein varies, however. Cone-shaped before it latches on to a cell, the protein changes into a short spear after it connects with its target, creating a major challenge for vaccine makers – designing and maintaining the shape of the spike protein in its cone-shaped form, when it can be effectively neutralized, so that the human immune system will recognize it.
On Feb. 19, 2020, McLellan and the team released a study (later formally published in the journal Science) that was the first in the world to address that thorny challenge.
The answer was in the works as soon as the genome sequence of SARS-CoV-2 was first revealed to the world on Jan. 10 by scientists in China. Mclellan’s lab began simulating the spike protein on the viral surface based on the molecular information provided.
Within two weeks, the team had used cryo-electron microscopy – the most advanced technology for visualizing biological structures – to take the world’s first picture of the spike protein and craft its first 3D molecular structure map.
Not only that, the team substituted two new proline (a compound of many proteins) molecules into the spike protein it was designing to give it an appearance identical to the cone-shaped spikes.
Experiments on animals conducted by a National Institutes of Health team led by immunologist Barney Graham proved that McLellan’s spike protein could trigger an immune response and create a high concentration of the neutralizing antibodies that prevented the virus from latching on to human cells.
Moderna, which developed the mRNA vaccine, was the first company to apply the spike protein developed by McLellan’s lab as the foundation of a COVID-19 vaccine.
Clinical trials in only 66 days
Under normal circumstances, it would take three to six years to get a vaccine to a Phase 1 clinical trial. But Moderna, which had never successfully developed a vaccine before, used only 66 days from the time the genome sequence was released to get to the initial trial stage, a new record.
Other American pharmaceuticals followed suit.
The mRNA vaccine co-developed by Pfizer and BNT replicates Moderna’s concept – using mRNA to send a message to human cells to produce their own spike proteins and stimulate an immune response. Johnson & Johnson’s adenovirus vaccine works by sending the spike protein’s DNA into a cell’s nucleus, which then copies the DNA into mRNA.
Novavax has taken somewhat longer to develop its vaccine, a protein subunit vaccine that purifies the spike protein in vitro and then injects it to stimulate immune cells. Unlike the mRNA vaccines, this type of vaccine directly introduces a purified fragment of the novel coronavirus (which cannot cause the disease) into the body to elicit a protective immune response.
 (Source: AP)
(Source: AP)
Regardless of their differences, all of these vaccines enable immune systems to learn how to identify the SARS-CoV-2 coronavirus and thwart any attacks.
Both the Pfizer-BNT and Moderna vaccines received emergency use approval in the United States in December 2020 based on data showing them to be highly effective against the virus, underpinned by the research done by McLellan and his team.
Old research comes in handy
McLellan’s career in deconstructing viruses actually began with his study of respiratory syncytial virus (RSV). This respiratory virus, most commonly seen in children under five, was as capricious as the SARS-CoV-2 virus, but McLellan found a way in 2013 to stabilize the shape of its protein, revolutionizing research into a vaccine for RSV.
He then turned his attention to the coronavirus family, which offered the same challenge, and began studying the HKU1 virus, a less infectious relative of the MERS and SARS viruses.
In 2017, McLellan and Wang Nianshuang, a postdoctoral researcher from China, discovered that adding two proline molecules could keep the spike protein shaped like a cone. They called it “S-2P” and patented it.
By then, however, the MERS and SARS epidemics had long ended and resulted in relatively few deaths. Thus, while academia was amazed by the team’s findings, pharmaceutical companies had little interest in using them to make vaccines.
Until COVID-19 arrived, that is.
When the novel coronavirus erupted, the team relied on its HKU1 research to quickly stabilize the shape of the spike protein that would mimic that of SARS-CoV-2. The patent that had been ignored was suddenly a hot commodity, and it led to vaccines that have saved countless lives.
McLellan said that after his team reconfigured their S-2P for the COVID-19 virus, they gave “the plasmid that expresses S-2P” (used to generate the protein) to over 100 labs around the world. The response led them to double down on their research.
“We quickly began receiving feedback that the protein was difficult to produce for many researchers. People from the Bill and Melinda Gates Foundation also reached out to say that their funded investigators were having problems and wondered whether we could improve upon this protein,” McLellan said.
HexaPro: Full of promise
McLellan enlisted Hsieh Ching-lin’s help to develop a better spike protein structure.
Guided by McLellan, Hsieh quickly found an improved approach that used six prolines in all – the two from the 2P spikes plus four additional prolines found elsewhere in the protein, according to the New York Times.
Not only was the new spike protein, called HexaPro, more stable, production capacity could increase nearly 10-fold, and smaller doses could generate the same amount of neutralizing antibodies, lowering the cost per dose.
“This is especially advantageous for the development of subunit vaccines,” McLellan said. The two Taiwanese vaccine makers that have applied for emergency use approval – Medigen Biotechnology and UBI Asia – are subunit vaccines, similar to the Novavax vaccine.
“You can freeze and unfreeze it three times, keep it at normal temperatures for two to three days or even heat it, and its shape won’t change. It’s a very good antigen,” Hsieh said of the new six-proline protein.
Some labs have found that HexaPro can be kept at room temperature for a week, leading them to conclude that it can be used for vaccines storable in similar conditions, in stark contrast to mRNA vaccines, which are stored at minus 20 degrees Celsius.
In July 2020, the team released the pre-print version of its study on HexaPro in which Hsieh was the lead author (formally published in Science in September 2020), and it caught the attention of pharmaceuticals.
But McLellan and the University of Texas also hope it will give low- and middle-income countries a chance to ease the severe shortages of COVID-19 vaccines many of them face.
According to the New York Times, the university has licensed companies and labs in 80 of those vaccine-starved countries to use HexaPro in their vaccines without paying royalties.
They will also be able to use the SARS-CoV-2 vaccine (NDV-HXP-S) developed with this new technology in cooperation with the Icahn School of Medicine at Mount Sinai that enables the coronavirus vaccine to be made the same way as flu vaccines have been made since the 1950s, by cultivating them in chicken eggs. One egg can yield between five and 10 doses.
In other words, even countries lacking biotechnology infrastructures can produce large volumes of inexpensive COVID-19 vaccines and get their populations inoculated as long as they have the equipment used to make flu vaccines.
Thailand was the first to register a Phase 1 clinical trial of the NDV-HXP-S vaccine in February, and Mexico, Vietnam and Brazil have all launched their own Phase 1 trials of similarly developed vaccines since then.
Shooting for the Holy Grail
Hsieh said McLellan is now leading the team to pursue a third-generation protein by continuing to mine the endless molecular permutations that exist.
“The goal is to create an antigen that can fend off all types of coronaviruses,” Hsieh said, envisioning the Holy Grail of the vaccine world.
Such a super vaccine could prevent the SARS and MERS coronaviruses that caused panic in many parts of the world, all variants of the current COVID-19 virus that continues to cause great suffering, and even the next coronavirus outbreak in the future.
What McLellan’s team has already achieved is seemingly impossible, providing the foundation for developing vaccines at record speed in a time of crisis. It cannot be chalked up to luck but rather to years of effort that offers a valuable lesson for the future, according to the UT professor.
“It is critical to invest in science and technology well before a pandemic occurs. Research takes years, or decades, and this work needs to be performed in advance. I hope the rapid development of efficacious COVID-19 vaccines demonstrates why it is critical to broadly fund basic science.”
Have you read?
♦ How far is Taiwan from herd immunity?
♦ Hsinchu Science Park’s pandemic response holds Taiwan’s economic lifeline
♦ Taiwan’s COVID-19 legacy depends on working from home and innovative testing
Translated by Luke Sabatier
Uploaded by Penny Chiang






